Stat Consult: Polyarticular Juvenile Idiopathic Arthritis – Clinical Advisor
Description
Polyarticular JIA is defined as chronic (>6 weeks) inflammatory arthritis in children <16 years old involving ≥5 joints during the first 6 months of illness2 subtypes:Rheumatoid factor (RF)-positive subtypeResembles adult rheumatoid arthritisSymmetrically affecting sma…….

Description
- Polyarticular JIA is defined as chronic (>6 weeks) inflammatory arthritis in children <16 years old involving ≥5 joints during the first 6 months of illness
- 2 subtypes:
- Rheumatoid factor (RF)-positive subtype
- Resembles adult rheumatoid arthritis
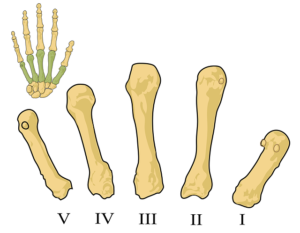
- Symmetrically affecting small joints
- Higher risk of rheumatoid nodules
- Overall poor functional outcome
- RF-negative subtype
- Typically asymmetric
- Higher risk of uveitis
- Fewer rheumatoid nodules
- Rheumatoid factor (RF)-positive subtype
Epidemiology
- JIA is one of the most common chronic diseases in children
- Reported prevalence of 3.8 to 400 cases per 100,000 children
- Reported incidence of 1.6 to 23 new cases per 100,000 children per year
- Approximate prevalence of International League of Associations for Rheumatology (ILAR) subtypes among children with JIA
- Oligoarticular 50%-60%
- Polyarticular 30%-35%
- Systemic-onset 10%-20%
- Psoriatic 2%-15%
- Enthesitis-related 1%-7%
- Reported frequency of polyarticular subtypes among all JIA
- 2%-7% for rheumatoid factor (RF)-positive polyarthritis
- 11%-28% for RF-negative polyarthritis
- Possible risk factors include
- Human leukocyte antigen (HLA) associations; increased likelihood for
- RF-positive polyarthritis with DRB1*04, DQA1*03, DQB1*03
- RF-negative polyarthritis with A2, DRB1*08, DQA1*04, DPB1*03
- Increased antibiotic exposure in infancy
- Human leukocyte antigen (HLA) associations; increased likelihood for
Etiology and Pathogenesis
- Complex disease with multiple environmental and genetic risk factors
- Cause of JIA appears to be breakdown in immunologic self-tolerance
- Increasing evidence for role of the microbiome (involved in immune system development/function)
- Changes in microbiome composition similar to those seen in other autoimmune diseases (type I diabetes, inflammatory bowel disease)
- Early exposure to antibiotics may increase risk via mechanism that alters intestinal microbiota
- Pathogenesis of synovitis and joint damage
- Inflammatory synovitis in JIA similar to synovitis in adult rheumatoid arthritis
- Inflammation prompts pannus formation, with cartilage and bone erosions mediated by degradative enzymes, such as metalloproteinases
- Complex role of genetics
- Role of genetic factors supported by
- Increased prevalence of autoimmunity among first-degree relatives of patients with JIA
- Reported monozygotic twin concordance rates (ranges from 25% – 40%)
- Human leukocyte antigen (HLA) region (encodes major histocompatability complex) is most important genetic contributor
- Many non-HLA regions reported to be associated with oligoarticular and rheumatoid factor (RF)-negative polyarticular JIA subtypes
- CD80-KTELC1 and JMJD1C -genetic associations not found in other autoimmune diseases; includes genes involved in
- T-cell development/activation
- regulating gene …….
- Role of genetic factors supported by