Tofacitinib Effective, Safe for Juvenile Idiopathic Arthritis – Physician’s Weekly
More data needed on long-term safety, but oral dosing, efficacy are positives in young patients
In young patients with polyarticular course juvenile idiopathic arthritis (JIA), tofacitinib—an oral Janus kinase (JAK) inhibitor—was effective, safe, and significantly reduced the …….

More data needed on long-term safety, but oral dosing, efficacy are positives in young patients
In young patients with polyarticular course juvenile idiopathic arthritis (JIA), tofacitinib—an oral Janus kinase (JAK) inhibitor—was effective, safe, and significantly reduced the number of flares by week 44 compared with placebo, according to results from the first phase III clinical trial to assess the efficacy of a JAK inhibitor in patients with JIA.
The results are published in The Lancet.
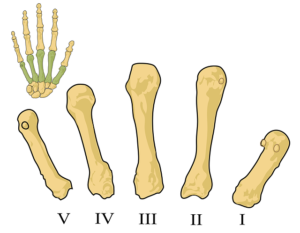
“Juvenile idiopathic arthritis (JIA) is a heterogeneous group of chronic conditions of unknown cause with onset occurring before the age of 16 years. Per current recommendations, patients with the most severe forms, polyarticular course JIA and systemic JIA, are treated with conventional synthetic and biological disease-modifying antirheumatic drugs (DMARDs), which have considerably improved long-term outcomes over the past 30 years,” wrote Nicolino Ruperto, MD, MPH, of IRCCS Istituto Giannina Gaslini, Genova, Italy, and colleagues from the Pediatric Rheumatology International Trials Organization and Pediatric Rheumatology Collaborative Study Group.
In this double-blind, withdrawal phase III study, Ruperto and colleagues included 225 young patients, ages 2 to ˂18 years, with polyarticular course JIA from 64 centers in 14 countries. In all, 82% of patients had polyarticular course JIA, 9% had psoriatic arthritis, and 9% had enthesitis-related arthritis. Most patients (65%) received concomitant treatment with methotrexate.
The mean age of these young patients was 13 years, mean age at diagnosis was 8 years, and mean disease duration was 2.5 years. Most patients were female (75%) and White (87%). The mean number of joints with active disease was 10.0, with a mean of 6.0 joints with limited motion. Mean CHAQ-DI score was 0.9.
During the initial phase of the study, patients received oral, open-label tofacitinib in doses based on weight (≤5 mg twice daily) for 18 weeks. For part two of the study, patients who reached a response of at least JIA/ACR 30 were then randomized to either continue tofacitinib or placebo for 26 weeks.
The primary endpoint of the study was JIA flare rate by week 44 during part two of the study.
By week 44, patients treated with tofacitinib had significantly lower flare rates than those treated with placebo, 29% versus 53%, respectively (HR: 0.46; 95% CI: 0.27-0.79; P=0.0031).
Adverse events occurred in 77% of patients treated with tofacitinib versus 74% of those treated with placebo, and serious adverse events occurred in 1% and 2%, respectively. The most common adverse events were upper respiratory tract infections (15%), disease progression (6%), and JIA exacerbation (4%). Temporary dose reduction or temporary treatment hold due to adverse events occurred in 11% of patients treated with tofacitinib compared with 9% of placebo.
In all, 48% of patients treated with tofacitinib developed infections or infestations. No deaths occurred.
Ruperto told BreakingMED: “JIA is a chronic condition and the most common cause of acquired disability in children. This study reported two major findings specific for JIA with polyarticular course (at least 5 joints with active arthritis), enthesitis-related arthritis and psoriatic arthritis—the possibility to have an effective and safe drug with a new mechanism of action that could be considered for patients who do not respond to other standard treatment, [and] this is the first oral drug (pills or syrup), which is an obvious advantage for children.”
One obvious advantage of tofacitinib over other treatments for JIA—including anti-TNF, anti-IL6, anti-B cell, and methotrexate that require subcutaneous or intravenous administration—is that it is an oral medication, stressed Ruperto.
But how does tofacitinib compare in efficacy? “There are no data related to a direct comparison with other treatments, but the different mechanism of action of this drug (a JAK inhibitor) increases the drug availability, especially for children who do not respond to other treatments,” Ruperto said.
“Generally clinical trials in JIA are related to the most frequent form which is called JIA with polyarticular course. In this case there are also initial, but limited, data on two more rare forms of JIA namely enthesitis-related arthritis (ERA, arthritis association with inflammation of the entheses the sites where tendons or ligaments insert into the bone) and juvenile psoriatic arthritis (jPSA, with arthritis plus psoriasis),” she added.
“Tofacitinib was the first JAK inhibitor to be licensed for rheumatoid arthritis in 2012, and since then JAK inhibitors have been increasingly used for immune-mediated disorders in adults. Their once or twice daily oral formulation makes them an attractive prospect for use in children. Furthermore, whereas the cost of biologics has reduced with the advent of biosimilars, small molecule JAK inhibitors still confer considerable price advantage, and therefore market accessibility, over biologics, particularly in low-income and middle-income countries,” wrote Sarah L.N. Clarke, BSC, BMBCh, research training fellow, and Athimalaipet V. Ramanan, MBBS, MSc, both of the Department of Pediatric Rheumatology, Bristol Royal Hospital for Children, U.K., in an accompanying editorial.
They noted that in these results from Ruperto et al, only four cases of serious infections occurred. However, an important limitation was the exclusion of children with uveitis.
“Uveitis is the most common and potentially serious extra-articular manifestation of JIA. It affects between 12% and 30% of patients and is a considerable cause of JIA-associated morbidity,” according to Clarke and Ramanan.
“Choice of biologic for methotrexate non-responders is often guided by uveitis status, with adalimumab having the best evidence for efficacy in both arthritis and uveitis. The study excluded patients with active uveitis within 3 months of enrollment and included only one participant with a history of inactive uveitis. Thus, evidence of the effect of tofacitinib on uveitis incidence or activity is not available and would be important in informing real-world treatment choices, both in polyarticular course JIA and more broadly,” they added.
Other study limitations, wrote Ruperto and colleagues, include the indirect assessment of the efficacy of tofacitinib according to the incidence of flares, the small study population that was primarily White, the inability to detect rare adverse events, and the need for more long-term safety data on tofacitinib in routine care.
“Despite its limitations, the trial by Ruperto and colleagues represents an important step in the treatment of JIA by providing the first indications of the efficacy of tofacitinib in JIA and addressing the need for a globally accessible, oral therapy. Moving forward, although JAK inhibitors appear to have a similar safety profile to biologics in adults, assessing the long-term safety profile of novel therapeutics in children is of high importance and underscores the needs to develop longitudinal, international disease registries in JIA to address and evaluate these concerns,” concluded Clarke and Ramanan.
-
In children with juvenile idiopathic arthritis (JIA), flare rate by week 44 was significantly lower with tofacitinib than with placebo.
-
Tofacitinib is a Janus kinase inhibitor that—unlike other approved treatments for JIA— offers the benefit of being an oral treatment, rather than subcutaneous or intravenous.
Liz Meszaros, Deputy Managing Editor, BreakingMED™
This study was funded by Pfizer.
Ruperto has received honoraria for consultancy fees or speaker bureaus from Ablynx, AstraZeneca/MedImmune, Biogen, Bristol-Myers Squibb, Boehringer Ingelheim, Eli Lilly, EMD Serono, F Hoffmann-La Roche, GlaxoSmithKline, Janssen, Merck Sharp and Dohme, Novartis, Pfizer, R-Pharm, Sanofi, Servier, Sinergie, and Sobi. The IRCCS Istituto Giannina Gaslini, where NR works as a full-time public employee, has received contributions from the following pharmaceutical companies in the past 3 years: Bristol-Myers Squibb, Eli Lilly, F Hoffmann-La Roche, GlaxoSmithKline, Janssen, Novartis, Pfizer, and Sobi; this funding has been reinvested for the research activities of the hospital in a fully independent manner, without any involvement of third parties.
Clarke receives support from the Wellcome Trust for a doctoral training fellowship.
Ramanan has received speaker’s fees, served on advisory boards, and received consulting fees unrelated to the topic of this Comment from AbbVie, Novartis, Roche, Swedish Orphan Biovitrum AB, and Union Chimique Belge, and serves on an advisory board or steering committee for Eli Lilly on trials of baricitinib in children with rheumatic diseases.
Cat ID: 68
Topic ID: 90,68,730,138,192,68,925
Source: https://www.physiciansweekly.com/tofacitinib-effective-safe-for-juvenile-idiopathic-arthritis/